@--------------------------------------------------------------
Chapter 2 Type classification of the cases
The author considers that the eruptions in the process of steroid withdrawal might be classified into several types. The patterns of eruption might adhere closely to the sensitivity to corticosteroids. Such individual differences are mentioned in the guidebook for allergic diseases published by Tokyo metropolis hygiene section in 1999.
It has been reported in the guidebook 'As for the sensitivity of the patient to topical steroids, there is an individual difference from the clinical observation. There is a steroid-allergic group which has contact dermatitis with steroids, a steroid-resistant group to which topical steroids becomes ineffective, a steroid-addicted group in which responds to steroids but worsens after interruption and a steroid-sensitive group in which steroids are effective and rapid aggravation is not observed. Steroid-allergic group is well known and confirmable by patch testing, while steroid-resistant group and steroid-addictive group are conceptual classifications based on the clinical efficacy. The method for identifying the groups has not yet been established.f
The 29 cases in this book may be classified into the steroid-resistant group or steroid-addicted group because topical steroids were effective but eruption relapsed soon after interruption. And case 27 belongs to steroid-resistant group because even the triamcinolone acetonide injection never responded.
On the other hand the steroid-sensitive group exists whose eczema is mild and coincides with the description in the classical textbooks of dermatology.
Probably the general practitioners are consulted mainly by this group. And dermatologists such as me who accept patients who refuse being treated by corticosteroids have less chance to see them.
If you had the impression that e I have never seen such eczematous patients. Are they really patients with atopic dermatitis? f from this book, that might be surely the difference among groups which we are familiar with.
However, as mentioned in the guidebook, the classification of the groups is based on the clinical observation. There is no objective method for distinguishing them although the establishment of such methods is the most important. In this chapter, from the authorfs observation, the eruptions are classified to five types. That is,
Type 1 Flush and plaque pattern
Type 2 Erythema fusing pattern
Type 3 Geographically diffusing pattern
Type 4 Fulminant pattern
Type 5 Prurigo diffusing pattern
As this classification is based on the pattern of eruption, it is not completely objective or scientific. There are cases that the author myself hesitates to apply this classification. If objective methods are established, such classification might have no meaning in the future. The author considers, however, pattern classification of eruptions should be essential to dermatology.
@--------------------------------------------------------------
Type 1 Flushed and plaque pattern
The lesion is characterized by poorly demarcated flushed plaques. In some severe cases, an entire body is flushed or erythroderma develops, the cutaneous findings are simple and rarely present pigmentation, prurigo or lichenification. When erythroderma develops, well demarcated flushed plaque frequently appears on the wrists or ankles. This type is regarded as nearly pure atopic dermatitis because it is observed also in patients with no use of steroids for a long time after withdrawal and babies or infants with little use of steroids. The flushed plaque may progress to exudative erythematous appearance in prolonged cases in which rebounds occur for months or over one year.
 |
(before / 1 week / 2 months)
Because of no history of prolonged treatment with topical steroids in the following case of the same type, the clinical coarse might be a natural healing process itself, which is common in infants or children rather than the results of steroid withdrawal.
 |
(before / 2 weeks / 2 months / 6 months
7 months / 1.5 years / 2 years)
Thus type 1 eruption is also seen as a recurrence long after withdrawal and often responds to elimination of aggravating factors such as bacteria, environment, food and emotional stress and so on.
Type2 Erythema fusing pattern
Small macular lesions with rather obvious demarcation spread to fuse to each other and disappear often after developing erythroderma. The lesion before the fusion may be either reddish ( erythematous ) or brown in color. The reddish lesion resembles urticaria or measles and the brown lesion resembles Type 3 eruption which will be mentioned as a geographically diffusing pattern on latter page. Type 2 is not characteristic to steroid withdrawal as neither is type1. Type 2 eruption can be developed in several months after the first aggravation after withdrawal subsided. However the second aggravation is not so severe as the first in most cases.
 |
(before / 2 months / 7 months / 12 months)
Type 2 is not specific on occasion of withdrawal as neither is type 1, but type 2 should be also regarded as a recurrence of atopic dermatitis. To be emphasized, however, the severity of the later aggravations is often less than that of the previous one. It is possible that the severity of the aggravation is amplified just after withdrawal from steroids. In that sense, this type also can be regarded as one of steroid dermopathy.
The eruption is developed often at first from the face and moves to the chest or upper extremities. In the case developing erythroderma, the eruption moves to the wrists, dorsal hands and lowew extremities in order. Sometimes severe edema is observed in the lower extremities.
Type3 Geographycally diffusing pattern
In this type an irregular and rather large geographical eruption gradually expands and diminishes. The eruption is a plaque with variegated reddish to brown color at first and becomes poorly demarcated as the diffusion progresses gradually. It vanishes after becoming a brown color predominant lesion or a brown pigmentation itself.
This type often responds to the disinfectant therapy. Erythroderma is rarely developed. Sometimes severe eczema on hands is accompanied in this type.
 |
(before / 1 week / 2 weeks / 1 month / 4 months)
The lesion is an irregular and geographical macule of which color is rather brown than reddish. The lesion expands and gradually diminishes. The above case is typical of this type, which often arises from the neck and gradually expands and diminishes.
The lesion of type 3 seems to hardly recur.
Even in occasions of recurrence, the lesions are liable to develope as papules or more poorly demarcated mild erythema which coincide with typical or classically described atopic dermatitis.
The dermatitis of type 3 is sometimes accompanied with severe eczema on hands though the reason is not obvious. It is a severe eczematous reaction with pustules and crusts and subsides with other eruption simultaneously or a little later.
 |
(before / 1 month / 2 months / 3 months)
Type 4 Fulminant pattern
Severe variegated eruption consisting of flushed plaque and other components such as exudates, crust, desquamation, pigmentation and excoriation develop in type4 between several weeks and one or two months after withdrawal. Rather rapid improvement is likely to follow between several weeks and months.
In most cases papules or prurigos which are resistant to steroids are scattered before withdrawal. The difference between type4 and type5 which is mentioned as prurigo diffusing pattern on later page lies in that type 4 is more furious. Sometimes body temperature exceeds 40 for seven to ten days. In most cases a sick leave or a temporary absence from school is necessary at the worst periods.
In spite of the severity of the systemic symptoms, the patients often reject suppressing them by temporal injection or resumption of steroids. Most patients seem to be aware that the condition is obviously caused by side-effect of steroids from their own experiences.
 |
(before / 2 weeks / 3 months / 7 months / 13 months)
Type5 Prurigo diffusing pattern
The prurigo is scattered on the whole body which shows almost normal appearance otherwise before withdrawal in type 5 though erythroderma is developed after withdrawal.
Prurigo or prurigo-like nodes flattens and remains as excoriation for a while. The progress is often persistant and long. It needs months or years till the rebound begins to subside. Much endurance is required of both the patient and therapist.
The type 5 pattern is characteristic to the withdrawal dermatitis the same as type 4 and it is different from a simple aggravation of atopic dermatitis.
 |
(before / 3 month / 7 months / 11 months / 19 months)
Chapter 3 Steroid skin syndrome in various skin diseases, but not in atopic dermatitis
The cases presented in this chapter are considered to be necessary for understanding the concept of so-called steroid skin syndrome, though they may deviate from the outline of this book, that is, steroid withdrawal in atopic dermatitis.
Steroid skin syndrome is the conditions in which stronger or more various aggravation of the eruption stemmed from discontinuation of application of steroids after long term use.
Such a condition can occur in a variety of skin diseases including atopic dermatitis as already described by Kligman in 1979.
The steroid skin syndrome is different from the classic adverse effects such as rosacea, acne or skin atrophy caused during application of the steroid ointment.
It is difficult to notice for the doctors because there is no symptom during application of steroid but symptom emerges for the first time after discontinuation of them.@(The patients notice this condition and by disbelief stop visiting the doctors who prescribing the steroid-containing ointment. Therefore, doctors hardly notice it.)
Rebound phenomenon after the continuous application of steroids to psoriasis has been described in the textbook. However, curiously there is few report of rebound phenomenon in atopic dermatitis, though@rebound phenomenon in atopic dermatitis are becoming a matter of the great importance.
The steroid skin syndrome is not limited to atopic dermatitis. Paradoxically, there are cases that secede easily from steroids without any rebound even if large amount of steroid is applied to skin.
It seems to be true that there is a group of patients who became easily@steroid-addicted after continuous application of steroid ointment, and the ratio of such patients is high in patients with atopic dermatitis.It resembles just like that there are persons who easily develop glaucoma by the steroids at a rate.
It may be possible to distinguish the patient who are prone to have steroid skin syndrome prospectively in the future.
1. Steroid skin syndrome in Hand Eczema
Though this type of steroid skin syndrome is not a mater of great importance at present, the author thinks that considerably potential cases are occurring.
It often happens to be true that serum IgE values were high and RAST scores were positive by blood test for studying atopic predisposition because the rebound phenomena were observed after steroid discontinuation.
 |
(before / 2 months / 3 months / 7 months)
@ The rebound eruption is limited only on hands in some cases, but it disappears after causing eczema in the arm or the elbow when the hand lesion is improved like this case.
There are cases in which continuous steroid-resistant eczema was limited to one finger at first, but it expanded to the arm and trunk after steroid discontinuation and then it caused the erythroderma. The rebound phenomenon also occurs in the part to which the steroid is never applied.
 |
(before / 2 months / 4 months / 6 months)
2. Steroid skin syndrome in Nummular Eczema
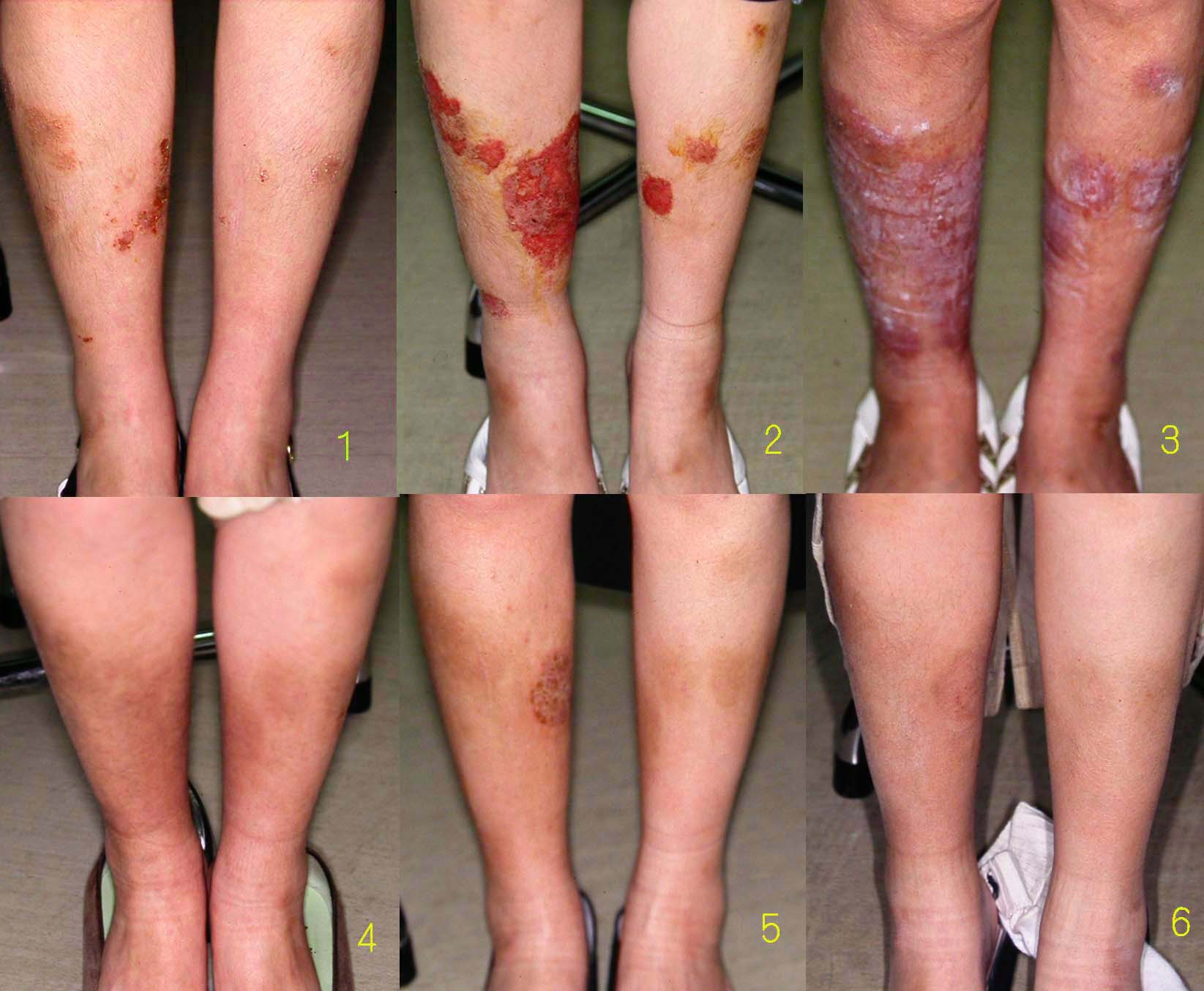 |
upper left: before (1 month after discontinuation : early stage of the rebound) upper middle: 1 months (middle stage) upper right: 2 months (later stage, the white material is zinc oxide ointment)
lower left: 4 months lower middle: 9 months (relapse of the nummular eczema) lower right: 14 months (almost cured by white petrolatum only not using steroids)
3. Steroid skin syndrome with Senile Xerosis
 |
(before / 2 months / 6 months / 10 months)
4. Steroid skin syndrome with Palmo-Planter Pusturosis
 |
(before / 1 month / 4 months / 5 months)
5. Steroid skin syndrome resembling Contact Dermatitis
 |
(before / 3 months / 5 months / 10 months)
@@@@@@@@@@